Regenerating Public Health
Making the case in less than 12 minutes: Malnutrition is our biggest challenge...
… and a Ruminant Revolution will be part of the solution. From my presentation to the Joint Southern & Western Sections Meeting of the American Society of Animal Science.
This post was created from the transcript from my presentation, with an assist from Grok.
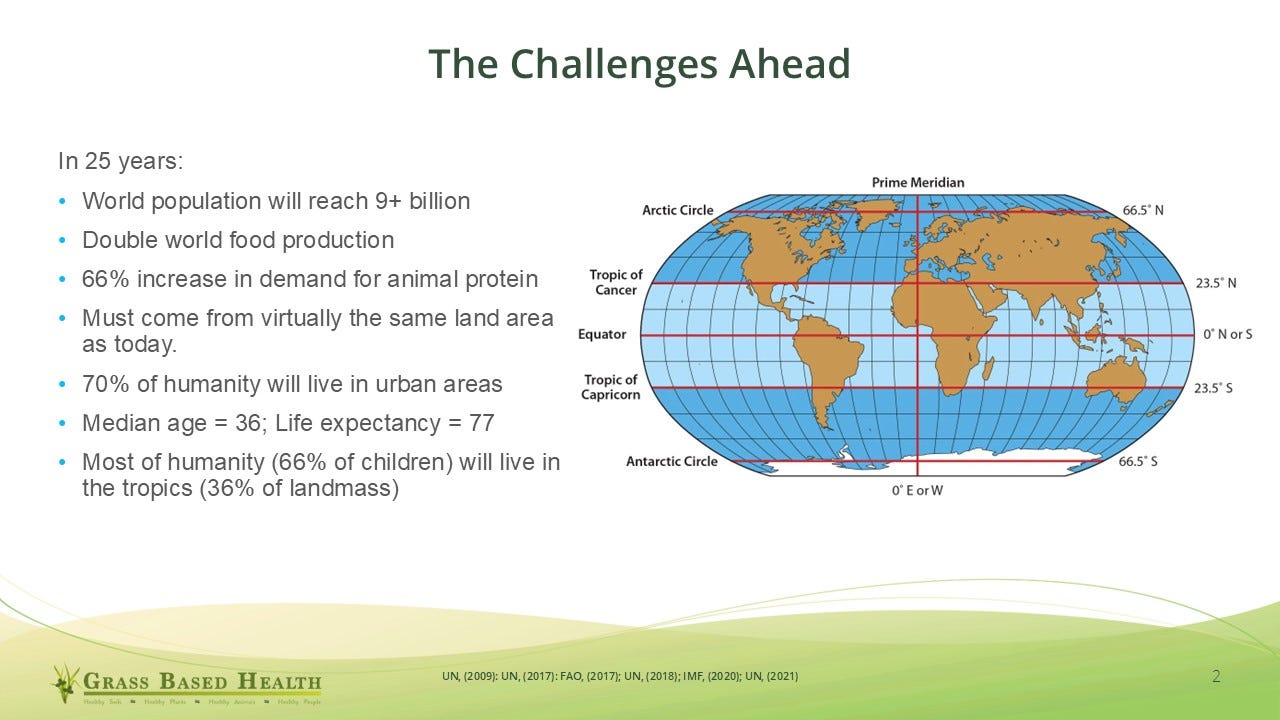
As we move further into the 21st century, it's important to reflect on the challenges that lie ahead. For those of you early in your careers, this is your professional lifetime and the challenges you might get to address. And while we face many global concerns, I believe an even more urgent issue demands our attention: the epidemic of chronic illness.
Today, 60% of U.S. adults have at least one chronic disease, and 40% have two or more. These conditions account for 90% of the nation’s $4.5 trillion in annual healthcare expenditures—and the situation is worsening. By 2050, the number of people aged 50 and older living with one or more chronic illnesses is expected to double, with a 90% increase projected for those with multiple conditions.
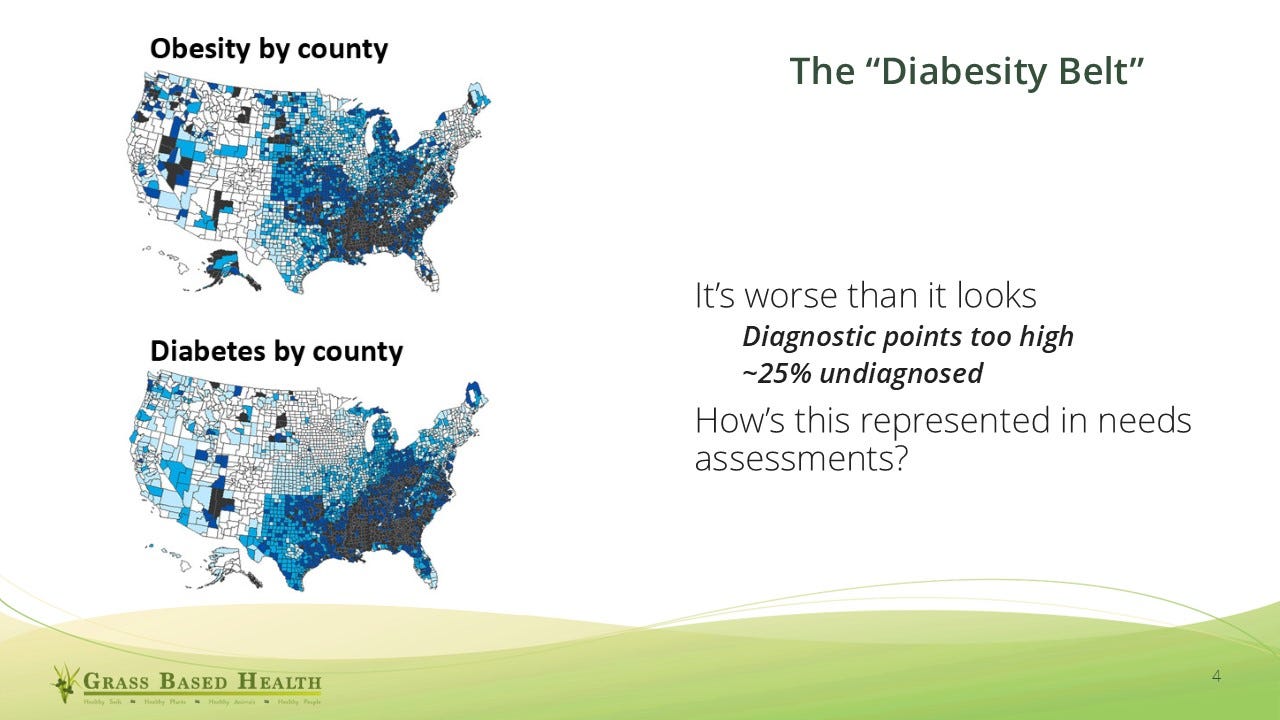
These trends are especially evident in what has been called the “diabesity belt”—a term coined to highlight the tight correlation between obesity and type 2 diabetes. The prevalence is likely even higher than reported, as many cases go undiagnosed, and our diagnostic thresholds may be set too high. Current research suggests we should begin to worry when A1C levels approach 5.5-6%, rather than the conventional 6.5-7% cutoff. This raises serious questions about how chronic illness is recognized in our communities and addressed in needs assessments.
The good news is that most chronic diseases share a common root cause: impaired metabolic function. As Professor Jeff Volek of the Ohio State University has observed, “Most chronic diseases have an underlying metabolic impairment as part of their pathophysiology.” Another researcher, Professor Benjamin Bikman of BYU, noted that insulin resistance “either explicitly causes the problem or exacerbates and accelerates it.” These insights, backed by extensive biomedical research, shift our understanding of chronic disease and highlight the importance of metabolic health.
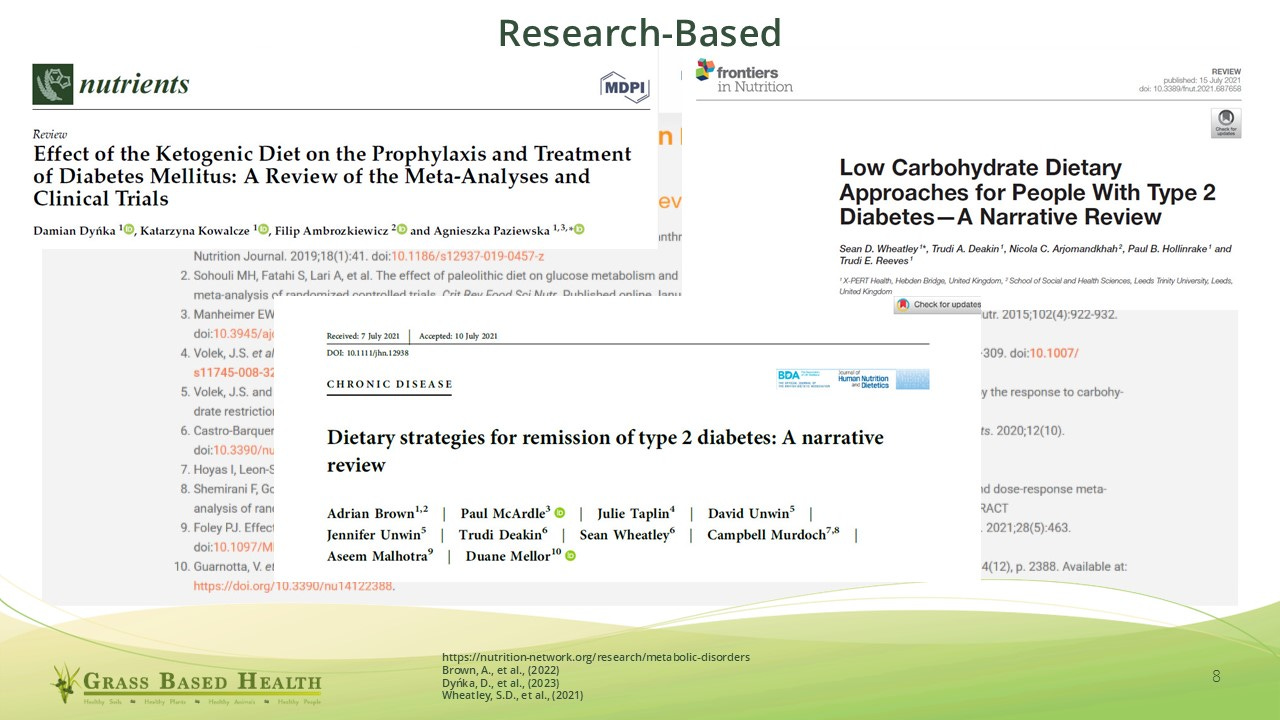
This growing body of evidence supports lifestyle medicine approaches that focus on metabolic restoration. For example, recent studies have shown that type 2 diabetes, long considered a chronic and progressive condition, can be placed into drug-free remission. That idea alone challenges decades of medical orthodoxy—and the language we use around disease matters. When we label diabetes as incurable, we shape expectations and outcomes accordingly.
Consider the example of malnutrition. Traditionally, it's been divided into undernutrition and overnutrition. But the term “overnutrition” supports the outdated “calories in, calories out” paradigm, which treats obesity as a cause of chronic disease. A better model, informed by current metabolic science, recognizes obesity as a marker of underlying metabolic dysfunction. The carbohydrate-insulin model suggests that excess fat accumulation—and many other chronic conditions—are symptoms of this deeper issue.
Adopting this broader definition of malnutrition reveals its true scope. Instead of affecting a few million people per year, malnutrition in its metabolic form may impact 60–70% of humanity. This reframing significantly elevates the urgency of the problem and demands a more strategic and inclusive response—from public health policy to agricultural investment.

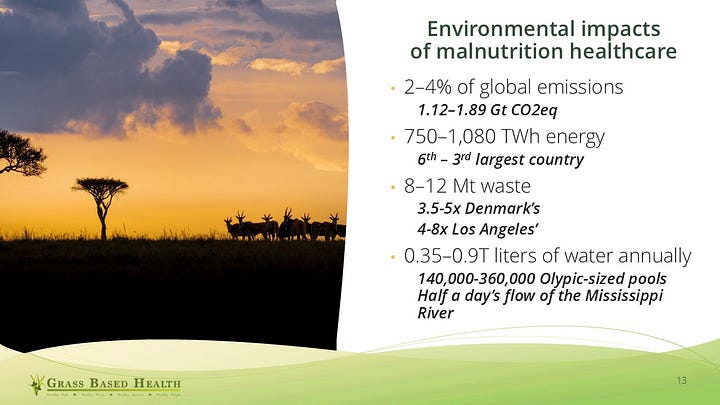
Malnutrition also imposes staggering economic costs. Global healthcare expenses attributed to it range from $5.8 to $6.5 trillion annually, encompassing both direct treatment and indirect societal impacts. In some regions, this burden restricts economic development. Yet, few realize the healthcare system’s environmental footprint: 2–4% of global greenhouse gas emissions stem from healthcare related to malnutrition—comparable to the 6% attributed to global beef production. These numbers underscore the need to reevaluate how we assess sustainability and environmental impact.
The World Health Organization has stated, “Death is inevitable, but a life of protracted ill health is not.” Their call for chronic disease prevention and control is essential, but it stops short of discussing remission or reversal. We must aim higher—to eliminate unnecessary suffering, especially when that suffering stems from preventable or reversible conditions. As stewards of agriculture and science, we have a role to play.


At its core, agriculture should be about increasing human flourishing. And flourishing requires nourishing. Around a fifth to a quarter of children under five globally are stunted due to a lack of essential nutrients—nutrients that are best or solely provided by animal-source foods. This developmental impairment lasts a lifetime and hinders national progress.
We must spread the message that food is not univocal. Calories are not interchangeable, and foods differ profoundly in their nutritional value. Many people today are overfed but undernourished. Some quantity of animal-source foods is essential for human development and long-term health—this is not controversial, it’s biologically grounded and defensible.

As a forage agronomist and advocate for ruminant agriculture, I believe our story—humanity’s story—runs from predator to steward. It bends back toward grass. Just as the Green Revolution addressed global caloric needs, we now need a Ruminant Revolution—one focused on delivering high-quality nutrition through environmentally wise, efficient systems.
In conclusion:
- We are experiencing a global epidemic of chronic illness rooted in hyperinsulinemia and insulin resistance.
- These are forms of malnutrition.
- Grassland agriculture, especially ruminant-based systems, offers part of the solution.
- We must work to improve productivity and sustainability worldwide.
What can you do? Educate yourself. Reach out—I’m happy to share information and connect you to the wider network of researchers and professionals engaged in this work.
What can our institutions do? What role might land-grant universities, the American Society of Animal Science, and the Cooperative Extension Service play in reshaping the public health conversation? These organizations are uniquely positioned to spread knowledge and improve lives.
Thank you for your attention and this opportunity. I welcome your questions now or anytime.
Brown, A., McArdle, P., Taplin, J., Unwin, D., Unwin, J., Deakin, T., Wheatley, S., Murdoch, C., Malhotra, A., Mellor, D., 2022. Dietary strategies for remission of type 2 diabetes: A narrative review. Journal of Human Nutrition and Dietetics. 35(1), 165-178. https://doi.org/10.1111/jhn.12938.
Dyńka, D., Kowalcze, K., Ambrozkiewicz, F., Paziewska, A., 2023. Effect of the Ketogenic Diet on the Prophylaxis and Treatment of Diabetes Mellitus: A Review of the Meta-Analyses and Clinical Trials. Nutrients. 15(3), 500. https://doi.org/10.3390/nu15030500.
Wheatley, S.D., Deakin, T.A., Arjomandkhah, N.C., Hollinrake, P.B., Reeves, T.E., 2021. Low Carbohydrate Dietary Approaches for People With Type 2 Diabetes—A Narrative Review. Frontiers in Nutrition. 8. https://doi.org/10.3389/fnut.2021.687658.






Keep up the good work.